The previous articles in this series showed how payers, providers, and digital health companies try to prove that they’re helping to create healthier...
MIPS
There’s fierce competition in the telehealth space, which is good because each company can approach telehealth from different angles and try out a...
To further support clinicians during the COVID-19 public health emergency, the Centers for Medicare & Medicaid Services (CMS) has extended the deadline for...
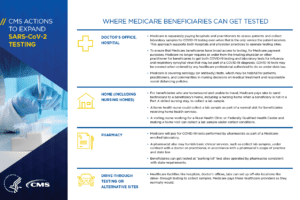
CMS continues to put out massive changes to regulations as they try their best to support healthcare during COVID-19. Yesterday, CMS came out with a bunch...
We previously shared that the MIPS program could be suspended or otherwise delayed. Today, CMS officially announced a delay to MIPS 2019 reporting which...
Given the fast moving nature of the COVID-19 and the changing virtual times, we’re going to try out some new changes here at Healthcare IT Today as well...
For what seems like an eternity, providers have been struggling with quality reporting requirements imposed by the MIPS program. Now, at long last, CMS seems...
On Monday, the Medical Group Management Association (MGMA) released the Annual Regulatory Burden Report at their Annual Conference. With responses from over...
It seems like an eternity that we’ve been writing about government regulations like Meaningful Use, HITECH, MIPS, MACRA, and a bunch of other...
In retrospect, we probably should have predicted that once Meaningful Use was put into place, some physicians would be better situated than others to take...